FACILITIES
-
Lab


Embryology Laboratory

Andrology Laboratory

Cryopreservation Laboratory

Genetic Laboratory

Embryology Laboratory
N.I.C IVF Clinic's Embryo Laboratory is certified to ISO Class 6 (Cleanroom Class 1,000) standards, meaning that the room contains no more than 1,000 particles of 0.5 microns or larger per cubic foot of air. The laboratory maintains strict environmental controls, including precise temperature, humidity, and pressure management.
A HEPA filter ensures the air is highly purified, reducing dust and pollutants. Non-UV lighting is used for the safety of embryos, and the laboratory operates under positive air pressure to prevent contamination.
At the entrance, an Air Shower system removes particles from staff clothing before entering the laboratory. Additionally, an interlock system between the operating room and the embryology laboratory ensures that only one door can be opened at a time, minimizing the risk of contamination between areas.
 Air Shower at the entrance of the Embryology LaboratoryN.I.C IVF Clinic's Embryology Laboratory provides the following services; Oocyte Retrieval, ICSI (Intracytoplasmic Sperm Injection), Embryo Culture, Embryo Biopsy, Oocyte and Embryo Vitrification, and Embryo Transfer. All tools and equipment are well provided with modern technology in order to provide the highest qualified work for Embryo Laboratory.
Air Shower at the entrance of the Embryology LaboratoryN.I.C IVF Clinic's Embryology Laboratory provides the following services; Oocyte Retrieval, ICSI (Intracytoplasmic Sperm Injection), Embryo Culture, Embryo Biopsy, Oocyte and Embryo Vitrification, and Embryo Transfer. All tools and equipment are well provided with modern technology in order to provide the highest qualified work for Embryo Laboratory. The equipment in Embryology Laboratory
The equipment in Embryology LaboratoryOocyte Retrieval
Transvaginal Ovum Aspiration is performed to retrieve eggs for fertilization. The collected eggs are transported through a pass box to the Embryo Culture Room. The tubes containing the eggs are placed in a tube warmer maintained at 37°C to preserve optimal conditions. The embryologist then examines the eggs in the IVF chamber, also maintained at 37°C. Additionally, the CO2 level is carefully controlled at 6% to maintain the temperature and pH of the culture environment as close as possible to the natural conditions of the human body.
 IVF Chamber
IVF Chamber Tube Warmer to maintain the eggs in the Pass box
Tube Warmer to maintain the eggs in the Pass boxThe Embryo Culture room is located IVFtech in work station area that is free from any contaminations. We have a HEPA filter to circulate and filter the air, so the air is cleaned and purified for the eggs and embryos. Also, we maintain the temperature at 37°C.
 Work station in the Embryo Culture room
Work station in the Embryo Culture roomICSI (Intracytoplasmic Sperm Injection)
In addition to conventional ICSI, the Oosight® imaging system is used to inspect the oocyte’s structure and visualize the meiotic spindle alignment. This allows embryologists to avoid damage or tearing of the oocyte during the ICSI procedure. Eggs fertilized using this technique show normal cell division and develop into healthy embryos.
 The examination's result and the image of Meiotic Spindle will show on the screen in work station
The examination's result and the image of Meiotic Spindle will show on the screen in work station ICSI process
ICSI processEmbryo Culture
The embryo culture process begins after the eggs have been fertilized with sperm in a workstation that provides optimal environmental conditions for embryo development. We carefully control factors such as gas composition, temperature, light exposure, nutrients, and pH to create an ideal environment for the embryos until they reach the blastocyst stage, which typically occurs 5–6 days after egg retrieval.
.jpg) Benchtop Incubator BT37
Benchtop Incubator BT37Benchtop Incubator BT37
The Benchtop Incubator BT37 provides optimal temperature, humidity, and pH conditions for embryo culture. Gas levels (Tri-Gas) and temperature can be quickly stabilized to ensure a consistent environment. The incubator is also equipped with an emergency battery system for backup power.
Embryo Transfer
The embryo transfer procedure is performed in a clean room (Class 1,000) to ensure a highly controlled environment. The transfer is carried out using a catheter within a sterile cabinet equipped with a HEPA filter to purify the air. The cabinet also has a system for air circulation and maintaining a stable temperature of 37°C.
 Sterile cabinet for containing embryos in the embryo transfer process
Sterile cabinet for containing embryos in the embryo transfer process
Andrology Laboratory
N.I.C IVF Clinic’s Andrology Laboratory has been certified according to ISO Class 7 (Cleanroom Class 10,000), which means the room contains no more than 10,000 particles per cubic foot of air measuring 0.5 microns or larger. Environmental controls are in place to maintain appropriate temperature, humidity, and pressure. Non-UV lights are also used to ensure the safety of sperm.

Workstation inside Andrology Laboratory
N.I.C IVF Clinic’s Andrology Laboratory offers the following services:
-
Semen analysis
-
Sperm freezing
-
Intrauterine insemination (IUI)
-
Surgical sperm retrieval: PESA and TESE
-
Sperm DNA fragmentation testing
-
MACS (Magnetic Activated Cell Sorting)
-
Microfluidic Sperm Sorting (MSS)
Semen Analysis
Semen analysis is a comprehensive assessment of semen quality. It involves visually examining the semen’s appearance, including color, odor, pH, viscosity, and liquefaction. The analysis also evaluates sperm concentration, motility, and morphology.
At our laboratory, semen is analyzed using a specialized instrument called Computer-Aided Sperm Analysis (CASA). The CASA system uses cameras to capture images of both motile and non-motile sperm. A computer program then calculates sperm concentration, the number of motile sperm, and other parameters to provide accurate and detailed results.
In addition, sperm morphology is assessed by capturing images of the patient’s sperm, allowing the laboratory to document and show the shape of the analyzed sperm to the patient.
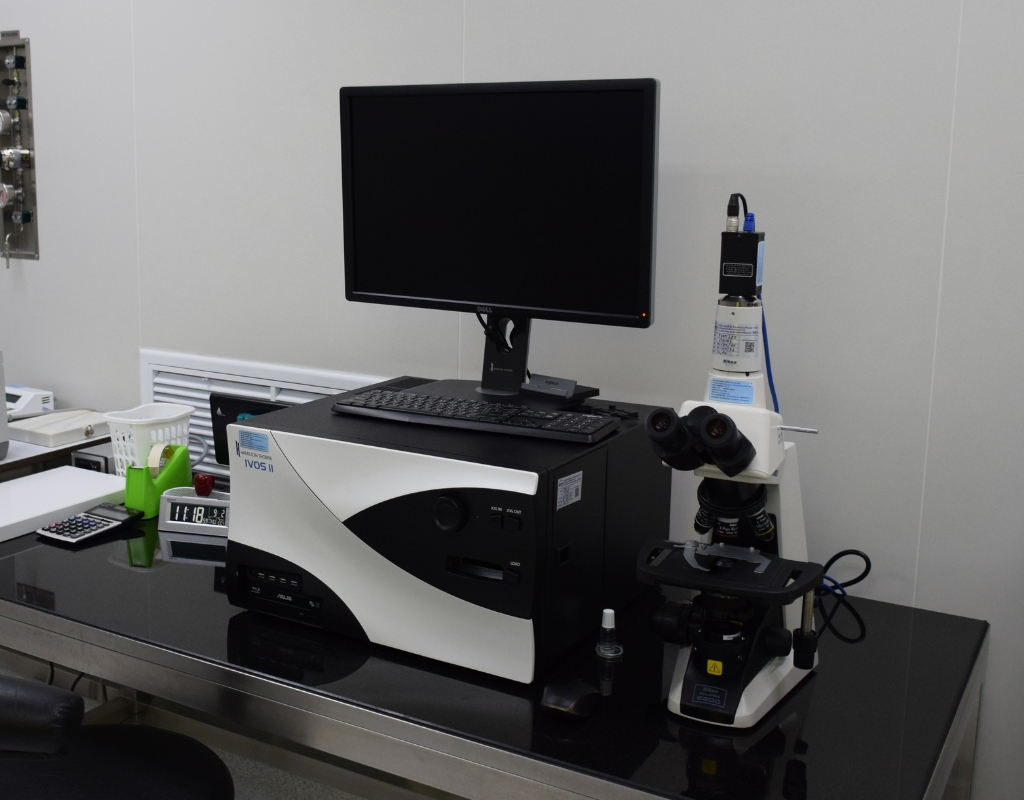
Computer-aided sperm analysis (CASA) machine
Halosperm G2
Halosperm G2 is a test that detects sperm DNA fragmentation using the Sperm Chromatin Dispersion (SCD) technique, which is both simple and accurate. Sperm are stained and examined under a bright-field microscope. Normal sperm with intact DNA form a halo around the head due to the presence of chromatin, whereas sperm without a halo have fragmented or damaged DNA.
DNA fragmentation in sperm can result from several factors, such as oxidative stress, a condition in which sperm are exposed to excessive free radicals. This can lead to changes in sperm structure and function, causing DNA breaks. High levels of sperm DNA damage are associated with lower fertilization rates, reduced embryo implantation, and an increased risk of miscarriage.
Sperm DNA fragmentation

Sperm DNA fragmentation
MACS Sperm
It is a method for selecting healthy sperm (Non-Apoptotic sperm). Based on the principle that sperm that are dead or have DNA damage (Apoptotic Sperm), epidermal cells will change their properties, causing Phosphatidylserine (PS) to move out to the outer sperm epidermal cells. Which is an indicator that the sperm quality is not quality. MACS GMP Annexin V reagent binds to dead or DNA damaged sperm well. which is coated with a magnetic substance as a sucker will trap the dead sperm to stick tightly can't run through Therefore, only healthy sperm will pass through this magnetic field and be able to continue using ICSI.

Magnetic bar and MACs GMP Annexin V set that is used for healthy sperm selection
Microfluidic Sperm Sorting (MSS)
Microfluidic Sperm Sorting (MSS) is an innovative technique for selecting high-quality sperm using a specially designed device with microfluidic channels. These channels replicate the natural sperm-selection process within the female reproductive tract. Only healthy, highly motile sperm with intact DNA can navigate through the intricate channels to the opposite side of the device, while weaker or DNA-damaged sperm are unable to pass through.
Unlike conventional sperm preparation methods, microfluidic sperm sorting selects sperm based on their intrinsic characteristics without the need for centrifugation, which is known to increase DNA fragmentation.
As a result, MSS yields sperm that are highly motile, fast-moving, free from debris and reactive oxygen species (ROS), and exhibit significantly lower levels of DNA fragmentation compared with other preparation techniques. These high-quality sperm are ideal for use in IUI, IVF, or ICSI, thereby improving fertilization outcomes, embryo quality, and overall treatment success rates.
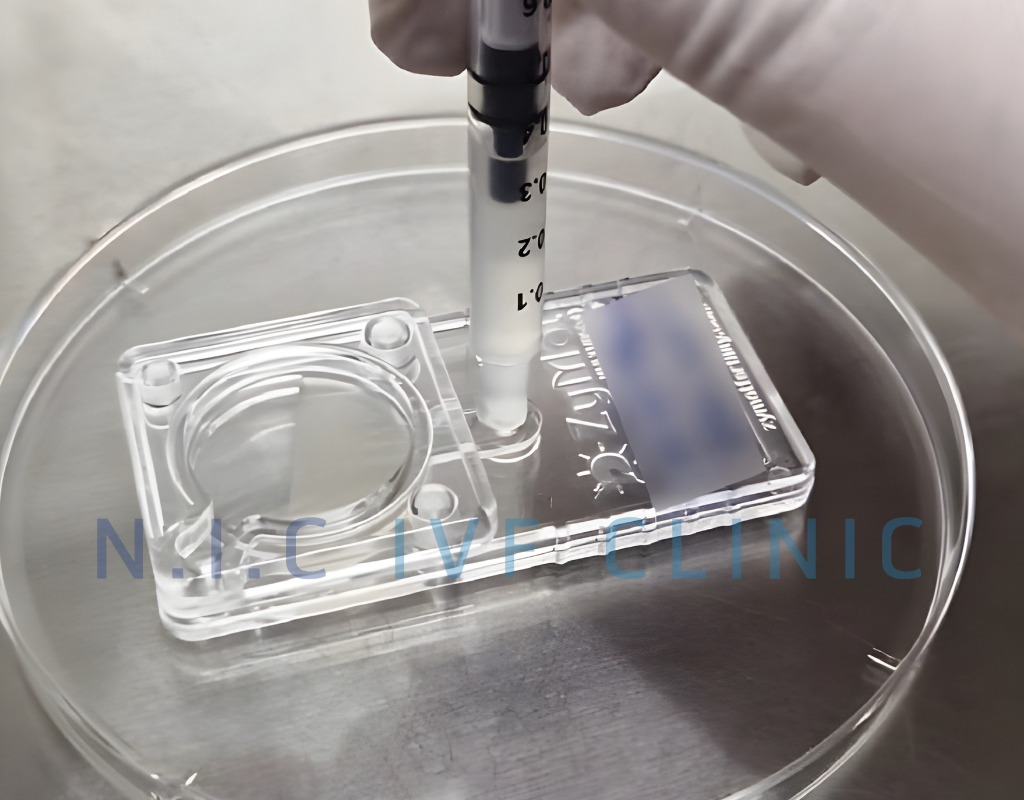
Microfluidic Sperm Sorting (MSS)

Cryopreservation Laboratory
N.I.C IVF Clinic's Cryopreservation Laboratory is separated from Embryology
Laboratory and Andrology Laboratory. Cryopreservation Laboratory has a system controlling pressure, temperature, and humidity. The laboratory also has been certified according to ISO Class 7 standard or Cleanroom Class 10,000 (Room with particle 0.5 Micron or larger but no more than 10,000 particles/1 cubic foot air). Furthermore, there is a security check system to control people who come in and out the laboratory. The storages for sperm, eggs, and embryos are to be locked at all time for safety. In addition, there is an Oxygen Sensor machine
in the room to check the level of Oxygen (O2). If the level of Oxygen is lower than the standard and is dangerous to the staff, the machine will make an alarm right away.
The security system of the Cryopreservation room
Oxygen Sensor
Oocyte and Embryo Vitrification
The technology of Oocyte and Embryo Vitrification is to use cryoprotectants with high intensity to prevent crystallization that can be very harmful to embryos. Using liquid Nitrogen, the temperature will go down as quickly as possible to -196 degrees Celsius. This process protects embryos from any contaminations that might come with liquid Nitrogen. We actually can keep the embryos in storage for a long time. Most importantly, we keep noninfectious eggs and embryos separated from the infectious ones to make sure there is no contamination. The service recipient can be assured that there is absolutely no contamination. For example, we separated the container with Hepatitis B from the normal ones. Therefore. the patients can be very sure in every process because of our highest safety policy.

The technology of Oocyte and Embryo Vitrification

Separate frozen eggs and embryo containers are infectious and non-infectious.
Sperm Freezing
The technique for preserving sperm under cryopreservation in a tank of liquid nitrogen at -196 degrees Celsius. It can be done by releasing water from the cell in order to prevent crystallization because crystallization can kill sperm and decrease the temperature by using Cryoprotectant Agents (CPAs). This technique can help us keep sperm for a very long time, and we also separate non-infectious containers from infectious ones.

Storing frozen sperm in frozen sperm storage tanks

Genetic Laboratory
N.I.C IVF Clinic's Genetic Laboratory has been certified according to ISO standard Class 7 or Cleanroom Class 10,000 (Room with particle 0.5 Micron or larger but no more than 10,000 particles/1 cubic foot air). There is an establishment of environmental control such as making sure to have appropriate temperature, humidity, and pressure. We use a HEPA filter to prevent dust and pollution, so the air in the room is highly purified. N.I.C IVF Clinic's Genetic Laboratory provides the following services; increasing the amount of DNA with PCR and Whole Genome Amplification (WGA)techniques, embryo chromosome screening with Next Generation Sequencing (NGS), Single gene disorder examination by using Direct genetic testing method, and using mini sequencing and Indirect genetic testing which come from the method of Linkage analysis.
Embryo Biopsy for Genetic Testing
Nowadays, embryo biopsy is usually performed at the blastocyst stage. The procedure involves removing 4–5 cells from the trophectoderm, the part of the embryo that will develop into the placenta during pregnancy. This process does not affect embryo development.
The procedure is performed in the laboratory using laser-assisted systems (LYKOS) and an inverted microscope, which are considered very safe and have no impact on embryo growth or viability.

How Trophectoderm is being removed with laser. The yellow circle represents the laser's radius.
Preimplantation Genetic Testing: PGT
Currently, the technology of Preimplantation Genetic Testing (PGT) has improved tremendously. This testing was done for the first time in 1980 by using the PCR method to increase the amount of DNA in the diseases that can be inherited through sex chromosomes. Due to some technical limitations, the testing could only reveal the gender of the embryo but did not identify genetic or chromosome disorders. In addition, choosing to remove embryos in the gender that did not show any symptoms of the disease or being a carrier may lose the other gender that could either be completely normal or have a serious disease. So, the abnormalities of each embryo cannot be found. Therefore, there must be a specific testing technique that can identify gender, genetic, and chromosome disorders. Nowadays, Preimplantation Genetic Testing has been developed to increase the amount of DNA and more precise testing techniques such as Comparative Genomic Hybridization (CGH), Next Generation Sequencing (NGS), real time PCR, and Karyomapping. Now, the Preimplantation Genetic Testing technique that is commonly used is Next Generation Sequencing (NGS).
Next Generation Sequencing (NGS) is a new technology that identifies base sequencing faster and can be used for embryo chromosome testing which covers 24 chromosomes all at once with 95-97% correct results. Presently, because we perform embryo testing during Blastocyst, we can obtain more cells and then gain higher precise outcomes. Besides testing for having less or more chromosomes, we can look for segmental aneuploidy in chromosomes while old techniques such as FISH and CGH cannot deliver the same results. Moreover. NGS technique can increase the success rate in pregnancy and reduce miscarriage to 50%
.jpg)
Next Generation Sequencing machine (NGS)
-
-
Rest area
-
Operating room
-
Consult room
-
VIP room